In 1984 I wrote algorithms, and created a programme and named it “PAT”, the Paediatric Assessment Tool. This was to help junior doctors (SHOs) to differentiate minor from serious illness that require hospitalisation. I understood the loop holes, and stopped validating this tool and started searching for alternative. This was long before Jerome Groopman mentioned about Algorithms in his book “How Doctors Think”
Dr. Jerome Groopman, in his book How Doctors Think, discusses the limitations of relying solely on algorithms and standardized protocols in medical practice. He argues that while these tools can provide a framework, they often fail to account for the complexities and nuances of individual patient cases. Groopman emphasizes that medicine is not a one-size-fits-all discipline; each patient presents unique symptoms, histories, and contexts that may not fit neatly into predefined categories. Overreliance on algorithms can lead to misdiagnoses and inadequate care, as they may not capture atypical presentations or rare conditions.
He advocates for a more personalized approach, where physicians use their clinical judgment, experience, and intuition alongside evidence-based guidelines to make informed decisions. This approach encourages doctors to remain open-minded, consider a broader range of possibilities, and engage in thorough patient communication to ensure accurate diagnoses and effective treatments.
Several experts have addressed the limitations of relying solely on algorithms for sharing healthcare information and making medical decisions. Dr. Jerome Groopman, in his book How Doctors Think, discusses how overreliance on algorithms can lead to misdiagnoses and inadequate care, emphasizing the importance of clinical judgment and personalized patient care.
Additionally, Dr. Ruha Benjamin has explored the ethical implications of medical algorithms, highlighting how they can perpetuate biases and inequalities in healthcare. She advocates for a more critical and equitable approach to integrating technology in medicine.
Furthermore, a study published in the Journal of Medical Ethics examines the ethical challenges of algorithmic decision-making in healthcare, emphasizing the need for transparency, accountability, and the integration of human judgment to ensure patient-centered care.
These perspectives underscore the consensus among healthcare professionals and ethicists that while algorithms can aid in medical decision-making, they should not replace the nuanced understanding and empathy that human clinicians provide
There are few alternative methods to offer care that go beyond rigid algorithms, emphasizing personalized care, holistic understanding, and active patient involvement. Here are some key approaches:
1. Dr Maya - Symptom-Based Classification Systems
- Dr. Maya’s method, which categorizes symptoms into color codes (Red, Blue, Green, Yellow), helps identify the severity and urgency of illnesses. This approach empowers patients to make informed decisions while allowing healthcare providers to focus on those needing immediate attention.
- Benefit: It aligns with human thinking, simplifies decision-making, and prioritizes patient needs.
2. Clinical Decision Support Tools with Flexibility
- These tools use guidelines as a framework but allow physicians to incorporate their clinical judgment.
- Benefit: Combines evidence-based medicine with the physician’s intuition and experience.
3. Shared Decision-Making Models
- Actively involve patients in their care by explaining their conditions, treatment options, and potential outcomes.
- Benefit: Empowers patients to take control of their health and fosters trust in the doctor-patient relationship.
4. Narrative-Based Medicine (NBM)
- Focuses on understanding the patient’s story, not just their symptoms. This approach considers emotional, psychological, and social factors influencing health.
- Benefit: Provides a holistic view of the patient, improving care quality and satisfaction.
5. Technology-Assisted Self-Diagnosis
- Programs like Dr. Maya integrate technology to help patients self-diagnose using combinations of symptoms, reducing unnecessary doctor visits while ensuring serious conditions get prompt attention.
- Benefit: Supports early detection and prevention without overwhelming healthcare systems.
6. Community-Centered Healthcare
- Engage local resources, like community health workers, educators, and patient advocates, to provide culturally sensitive, localized care.
- Benefit: Reduces disparities in healthcare access and outcomes.
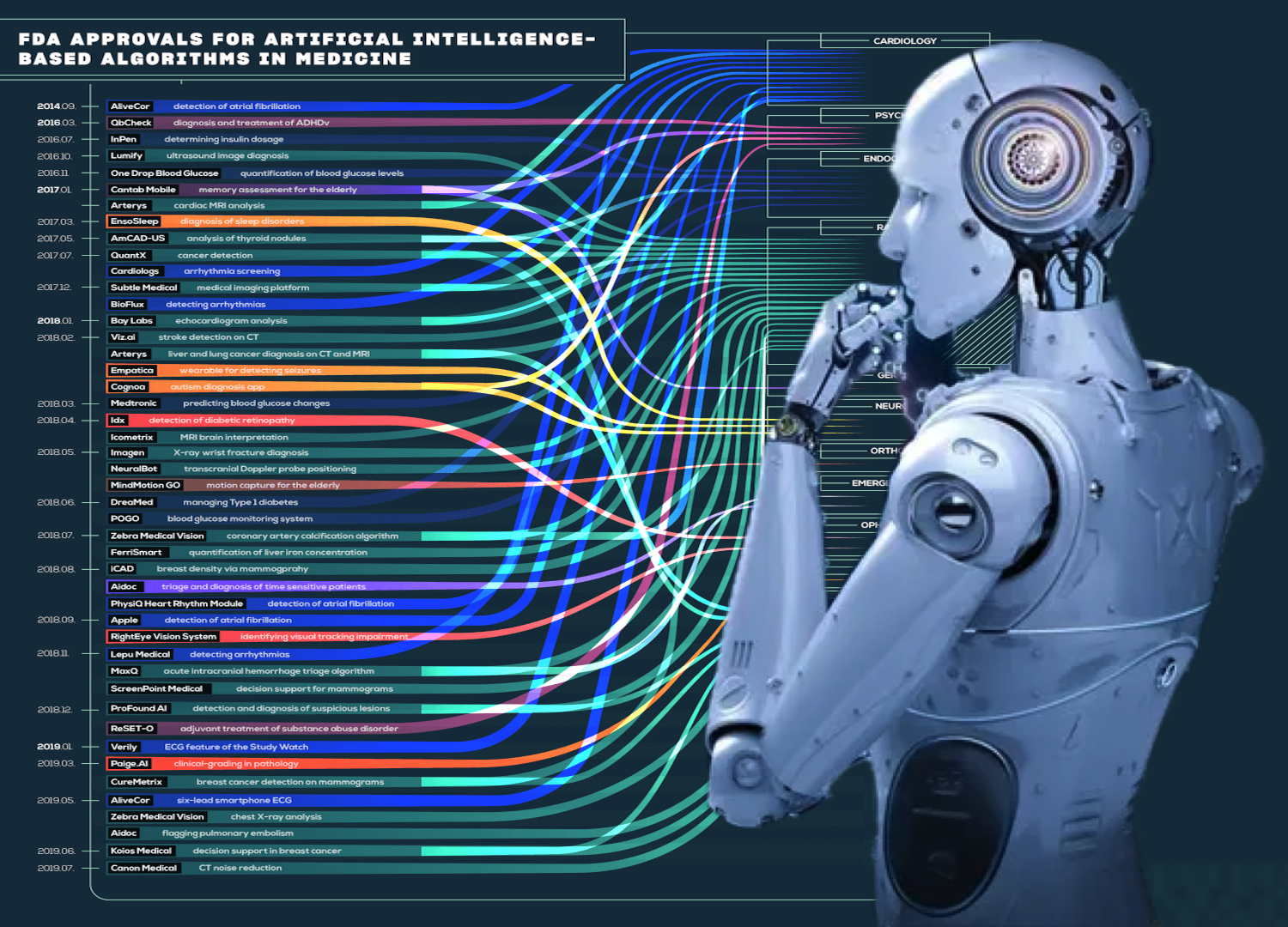
7. Integration of Artificial Intelligence with Human Oversight
- AI can assist in pattern recognition and data analysis but must be used with clinical judgment.
- Benefit: Improves efficiency without losing the human touch.
8. Focus on Preventive Care and Education
- Equip patients with knowledge about their health through workshops, apps, and accessible materials.
- Benefit: Encourages proactive health management and reduces dependency on medical professionals.
The Goal: Personalized and Ethical Care
A patient-centered approach means tailoring care to each individual’s needs, circumstances, and preferences while ensuring dignity, respect, and trust. By combining innovative tools like Dr. Maya with the empathy and expertise of healthcare providers, we can achieve a balanced, effective alternative to rigid algorithms.